There are two ways in which nanotechnology may be able to extend our lives. One is by helping to eradicate life-threatening diseases such as cancer, and the other is by repairing damage to our bodies at the cellular level – in essence, a nano version of the fountain of youth!
There are two ways in which nanotechnology may be able to extend our lives. One is by helping to eradicate life-threatening diseases such as cancer, and the other is by repairing damage to our bodies at the cellular level – in essence, a nano version of the fountain of youth!
Our average lifespan has been increased over the last 100 years by reducing the impact of life-threatening diseases. For example, vaccines have virtually eliminated smallpox. The application of nanotechnology in healthcare is likely to reduce the number of deaths from conditions such as cancer and heart disease over the next decade or so. There are many research programs working on these techniques;
Let’s look at the type of nano work that is currently being done in the way of eradicating cancer, one of the most serious of diseases on our planet:
An intriguing cancer treatment uses one nanoparticle to deliver a chemotherapy drug and a separate nanoparticle to guide the drug carrier to the cancer tumor. Nanorods circulating through the bloodstream exit where the blood vessels are leaking at the site of cancer tumors. Once the nanorods accumulate at the tumor they are used to concentrate the heat from infrared light, heating up the tumor. This heat increases the level of a stress related protein on the surface of the tumor. The drug carrying nanoparticle (a liposome) is attached to amino acids that bind to this protein, so the increased level of protein at the tumor speeds up the accumulation of the chemotherapy drug-carrying liposome at the tumor. Magnetic nanoparticles that attach to cancer cells in the blood stream may allow the cancer cells to be removed before they establish new tumors.
Read more about nanotechnology and its use in detecting and treating cancer
Another major killer in our time is heart disease. In this area, there are several efforts going on:
Researchers at the University of Santa Barbara have developed a nanoparticle that can deliver drugs to plaque on the wall of arteries. They attach a protein called a peptide to a nanoparticle which then binds with the surface of plaque. Studies have verified that the peptide attaches the nanoparticle to plaque. The researchers plan to use these nanoparticles to deliver imaging particles and drugs to both diagnosis and treat the condition.
Read more about this study of nanotechnology and heart disease
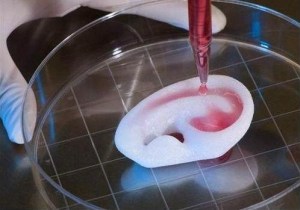
Perhaps the most exciting possibility exists in the potential for repairing our bodies at the cellular level. Techniques in Nanorobotics are being developed that should make the repair of our cells possible. For example, as we age, DNA in our cells is damaged by radiation or chemicals in our bodies. Nanorobots would be able to repair the damaged DNA and allow our cells to function correctly.
This ability to repair DNA and other defective components in our cells goes beyond keeping us healthy: it has the potential to restore our bodies to a more youthful condition. This concept is discussed by Eric Drexler, Ph.D., an established researcher and author whose work focuses on advanced nanotechnologies and directions for current research.
Drexler states: “Aging is fundamentally no different from any other physical disorder; it is no magical effect of calendar dates on a mysterious life-force. Brittle bones, wrinkled skin, low enzyme activities, slow wound healing, poor memory, and the rest all result from damaged molecular machinery, chemical imbalances, and mis-arranged structures. By restoring all the cells and tissues of the body to a youthful structure, repair machines will restore youthful health. ”
Maria Konovalenko
SCIENCE FOR LIFE EXTENSION FOUNDATION
http:/mariakonovalenko.wordpress.com/
maria.konovalenko@gmail.com